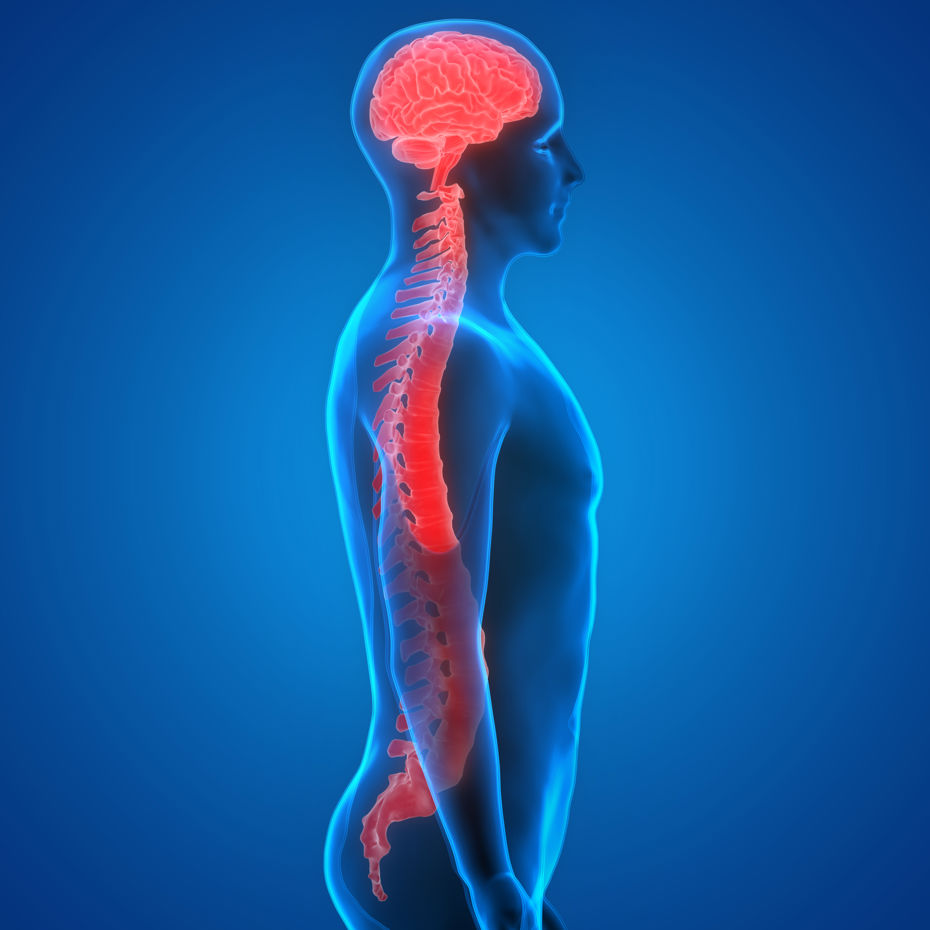
Neurogenic bladder is a disorder of the lower urinary tract created by damage to or diseases of the nervous system.
Problem

Found in many patients with neurologic disorders, including multiple sclerosis, Parkinson’s disease, spinal cord injury, and spina bifida among others, neurogenic bladder can lead to problematic symptoms and complications including urinary incontinence, frequency, and urgency, along with risk for infection and involvement of the upper urinary tract and kidney disease.
The disorder can also create substantial embarrassment resulting in social isolation for affected patients.
Damage to or diseases of the Central Nervous System (CNS) or within the peripheral or autonomic nervous system may lead to neurogenic bladder dysfunction. This dysfunction may arise as a result of several neurologic conditions and has been found in 40% to 90% of patients in the United States with multiple sclerosis (MS), 37% to 72% of patients with Parkinsonism, and 15% of patients with stroke.
It is estimated that 70% to 84% of patients with spinal cord injuries have at least some degree of bladder dysfunction. Bladder dysfunction is also frequently seen in patients with spina bifida, with vesicoureteral reflux present in up to 40% of children affected by 5 years of age and with up to 60.9% of young adults with spina bifida experiencing urinary incontinence.
Bothersome urinary symptoms associated with a neurogenic bladder include urinary incontinence (UI), frequency, and urgency. Patients also may have an increased risk and incidence of urinary tract infections (UTIs) and bladder outlet obstruction.
Management and treatment
Neurogenic bladder treatments can include behavior modification, pelvic floor muscle exercises, electrical stimulation, drug therapy, catheterization, or sometimes surgery.
Behavior modification, also called timed voiding or bladder retraining, can reduce problems caused by an overactive bladder. It combines willpower and exercise. The patient is asked to keep a voiding diary, which is a daily record of the amount and time of fluid intake, times of urination, and episodes of leakage. The rationale is to gradually increase the amount of time between voids, and in achieving a larger bladder capacity; episodes of urgency and urinary frequency, and nocturia will improve. It should take approximately 4 weeks for a bladder retraining program to work – if it is going to be appropriate for that individual.
Electrical-stimulatory therapy. Electrical stimulation is used in the treatment of stress incontinence, urge incontinence, and mixed incontinence. Can also be used for bladder emptying difficulties caused by weak micturition reflex and underactive detrusor. The purpose of the electrical stimulation is to strengthen the function of the normal nerves to control the bladder function.
It is important to know that there are several different options in electrical stimulation, such as TENS, IVES, Sacral neuromodulation, and SARS.
Drug therapy. There are as yet no drugs that target specific muscles such as the sphincter. However, there are classes of drugs that reduce muscle spasms and tremors and other drugs that might induce contractions. These can sometimes be effective in appropriate neurogenic bladder conditions.
Catherization. Catheterization is used to ensure complete bladder drainage, this can be either intermittent or indwelling.
Urinary diversion creates a stoma (opening) through which urine is diverted to a collection pouch.